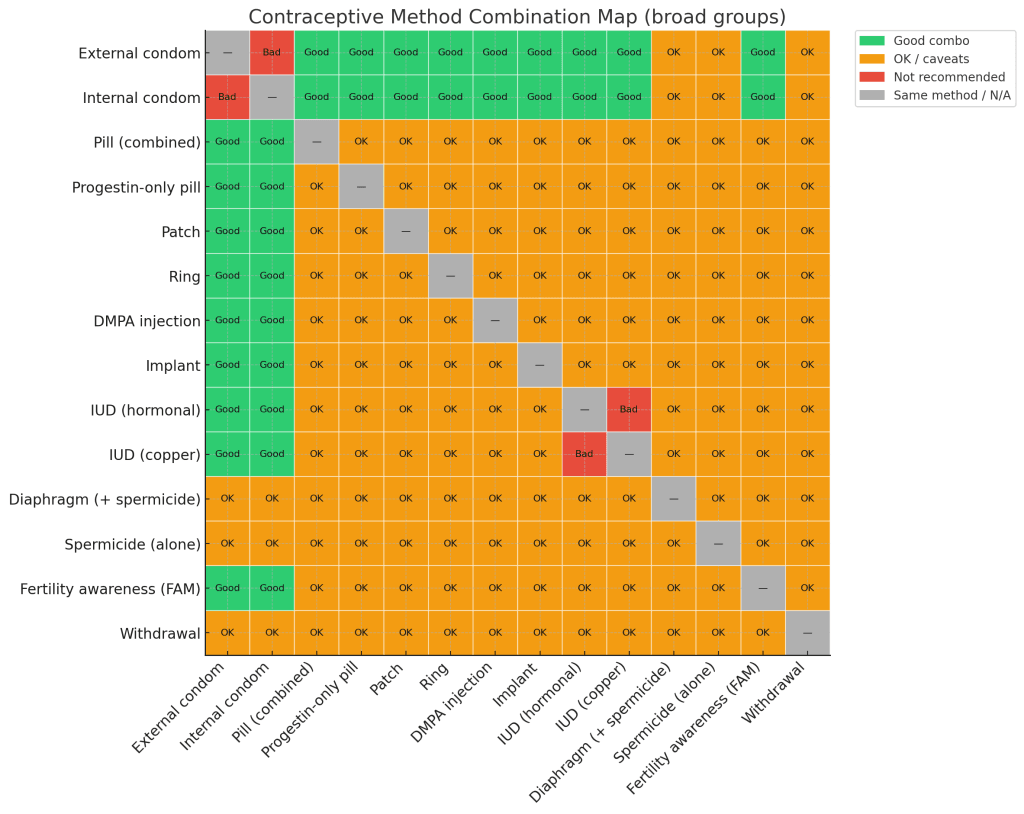
Some people choose to use more than one birth control method at the same time. This page summarises combinations that expert guidance from organisations such as the CDC and WHO generally considers reasonable for lowering pregnancy risk, while keeping STI protection in mind. The best combination for you depends on your health history, medicines, and preferences, so it is important to discuss options with a clinician.
The chart on this page shows a simplified map of how broad method pairs are usually classified (good combinations, combinations that are generally OK but need caveats, and pairs that are not recommended). It is only a visual overview and does not replace clinical judgement or the detailed guidance found in the sources listed below.
If you would like to see approximate numbers for specific pairings, you can use the Combined Contraceptive Effectiveness Calculator as an educational tool.
How combined effectiveness works (in plain English)
Each method has a chance of failure over a given time period. When two different methods are used together, pregnancy usually occurs only if both methods fail around the same time, so the overall risk can become lower. In real life this is an approximation. Some behaviours affect both methods at once, and combining certain hormonal methods may increase side effects without adding much benefit, which is why plans to stack hormonal methods should be reviewed with a clinician.12
Common pairings that often make sense
1) Pill plus condom
- Why many clinicians like this pair: The pill mainly works by preventing or disrupting ovulation. A condom adds a physical barrier and helps reduce the risk of many STIs.23
- Good fit: You want a daily method and also want STI protection or extra reassurance about pregnancy risk.
- Safety note: If pills are missed or a condom slips or breaks, clinicians often suggest considering emergency contraception and checking whether a pregnancy test will be needed later.
2) Hormonal IUD or implant plus condom
- Why: Long acting reversible contraception (LARC) such as hormonal IUDs and implants are among the most effective reversible methods. Adding a condom gives STI protection and an extra barrier if something unexpected happens.23
- Good fit: You prefer a method that does not need daily action, but you or your partner also want protection from many STIs.
3) Copper IUD plus condom
- Why: A copper IUD gives long term, hormone free pregnancy prevention. Condoms add protection against many STIs and provide a second barrier.23
- Good fit: You prefer to avoid hormones yet still want highly effective contraception and STI risk reduction.
4) Fertility awareness with training plus condom
- Why: When fertility awareness methods (FAM) are learned from a trained educator and followed closely, some couples use condoms or abstain during the estimated fertile days to reduce pregnancy risk further. Condoms add a barrier and some STI protection.4
- Good fit: Couples who can commit to careful tracking and are comfortable with the higher typical use failure rates that FAM can have compared with methods such as IUDs, implants or the pill.
When to consider emergency contraception
If a condom slipped or broke, a pill was missed, or a method was not used as planned during a time that might be fertile, emergency contraception (EC) may lower the chance of pregnancy. EC works best the sooner it is used. A doctor, nurse or pharmacist can help you choose between options and check for any medical reasons to avoid a particular product.
The Emergency Contraceptive Pill Effectiveness Calculator can give a rough idea of how timing may affect estimated risk, but it does not replace personalised advice from a clinician.
Check your combined protection
You can enter two methods and choose typical or perfect use settings in the Combined Contraceptive Effectiveness Calculator to see an approximate combined effectiveness for educational purposes.
Select your methods to see their combined effectiveness.
Quick safety notes
- STIs: Only condoms (external or internal) provide meaningful protection against most STIs, including HIV, when used consistently and correctly.6
- Spermicides: Products containing nonoxynol 9 can irritate genital tissue and are not recommended for STI or HIV prevention. Frequent use may increase HIV risk in people who are exposed to the virus.78
- Stacking hormones: Using more than one hormonal method at the same time is not routinely recommended and may not add much extra protection. Talk with a clinician before combining hormonal methods so that benefits and side effects can be weighed for your situation.2
FAQ
Which two birth control methods are often used together?
Many clinicians are comfortable with combinations that pair a highly effective method such as an IUD, implant or pill with a condom. The long acting or hormonal method provides strong pregnancy prevention, and the condom adds STI protection and a second barrier. The best combination for you should be chosen with a clinician who knows your medical history.
If you are curious about approximate numbers, the Combined Contraceptive Effectiveness Calculator can be used as an educational tool.
Should I use two condoms at the same time?
No. Using two external condoms together, or an external and internal condom at the same time, is not recommended. The extra friction can cause tearing, which increases the risk of pregnancy and STIs.
What should I do if a condom slips or a pill is missed?
Clinicians usually recommend considering emergency contraception as soon as possible and checking whether a pregnancy test will be needed later. A doctor, nurse or pharmacist can help you choose the right EC option and advise about ongoing contraception. You can also review typical timing using the Emergency Contraceptive Pill Effectiveness Calculator, which is for education only.
Sources
- Trussell J. Contraceptive failure in the United States. Contraception. 2011. (Typical vs perfect use failure rates.) ScienceDirect
- CDC. U.S. Selected Practice Recommendations for Contraceptive Use, 2024. MMWR Recommendations.
- CDC. Condom use and prevention resources. (Correct and consistent use reduces risk.) Condoms and HIV Prevention.
- CDC. Effectiveness of contraceptive methods (overview table). PDF.
- WHO aligned Family Planning Handbook. What condom users should not do (do not use male and female condoms together). Link.
- WHO Fact Sheet. Condoms. (Condoms can help prevent many STIs and unplanned pregnancy when used correctly.) Link.
- CDC STI Guidelines. Primary Prevention Methods. (Nonoxynol 9 in condoms adds no STI benefit.) Link.
- WHO News Release. Nonoxynol 9 ineffective for HIV prevention; frequent use may increase risk. Link.
This page is general information only and is not medical advice. For personal recommendations, talk with a doctor, nurse or clinic that knows your medical history.