Reviewed by Dr. Grace Ramosena, MBChB on Jan 25, 2026
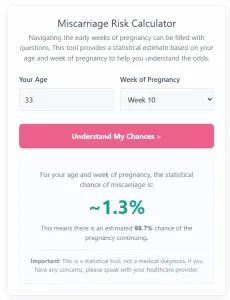
Estimate miscarriage risk by week and day. For the most accurate assessment, please include your maternal age, heartbeat status, prior history, and BMI.
Loss after 20 weeks is clinically defined as Stillbirth, not miscarriage. Please use our dedicated calculator for this stage.
Go to Stillbirth Risk Calculator →Based on Week Day :
Scope: This estimates the risk of loss from today up to 20 weeks. Loss after 20 weeks is medically classified as stillbirth. See Stillbirth Risk Calculator. Or to see your combined miscarriage and stillbirth odds, use our Chance of Live Birth Calculator.
Note: This tool uses statistical averages adjusted for age, history, and BMI. Every pregnancy is unique. Please consult your healthcare provider for medical advice.
How to use this calculator
- Enter your age: type your age in years.
- Enter your gestational age: add the week number and the day number (0-6), e.g., 8 weeks, 3 days.
- Optional advanced inputs: open Advanced options to add heartbeat status, prior miscarriages, prior live births, and BMI (via height and weight).
- Get your estimate: press Calculate to see the percent risk and the chance of continuing.
This tool is for education only and does not replace care from your clinician.
The Science Behind Miscarriage Risk
Most early miscarriages are due to chromosomal issues in the embryo, not anything a person did or did not do. The risk changes rapidly in early pregnancy and generally declines as gestational age increases.
- 1
Day-by-day baseline (what the calculator shows)
The estimate starts from a published day-by-day curve (about 3 to 20 weeks). For dates outside that range, the curve is smoothly extended to provide a reasonable estimate. Results are bounded between 0.1% and 99% to avoid over-certainty.
- 2
After a confirmed heartbeat
Once a fetal heartbeat is seen on ultrasound (often around 6-7 weeks), the ongoing risk is typically lower at the same gestational age. The day-by-day curve captures this general decline across the first trimester.
- 3
Optional factors
You can add prior miscarriages, prior live births, and BMI (from height and weight). These factors can nudge the estimate up or down based on population-level associations.
- 4
About age
Maternal age is an important population-level factor in miscarriage risk. The baseline day-by-day curve reflects average risk across ages; we’re exploring age-specific curves for future updates.
This calculator provides a statistical snapshot for a given day of pregnancy. It is for education only and does not replace care from your clinician.
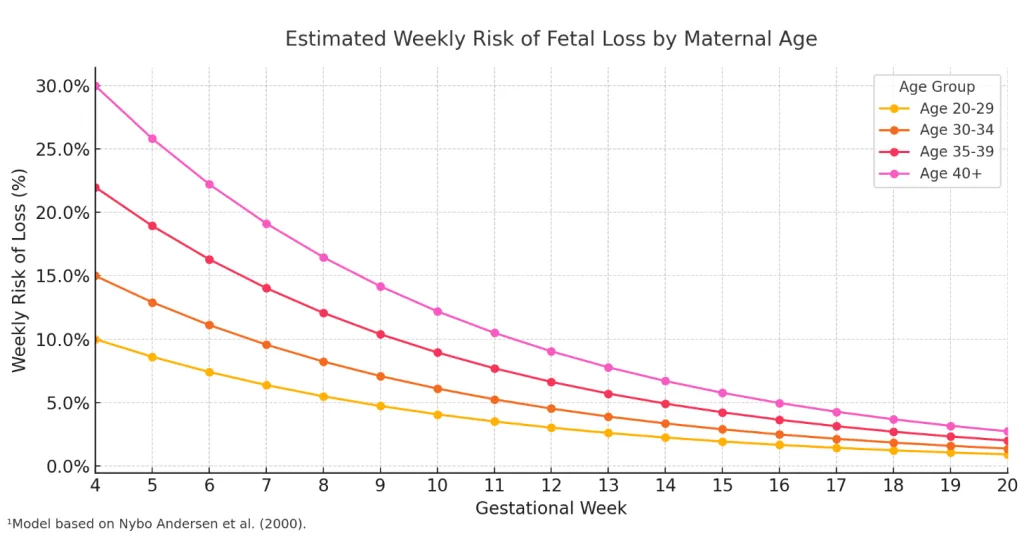
¹The data model is based on findings from a landmark study on fetal loss: Nybo Andersen, et al. (2000). Maternal age and fetal loss: a population-based register-linkage study. BMJ, 320(7251), 1708-1712.
Frequently Asked Questions
What week has the highest miscarriage risk?
Risk is highest in the very early stages of pregnancy (chemical pregnancy). Clinically, most losses occur before 12 weeks, with a significant drop in risk typically observed after Week 8.
Does seeing a heartbeat lower the risk?
Yes, significantly. Studies show that once a viable fetal heartbeat is detected on ultrasound (usually after 6-7 weeks), the risk of miscarriage drops to below 5-10% for most age groups. Use the "Advanced Options" in our calculator to see this adjusted risk.
I am spotting. What should I do?
Light spotting can be normal in early pregnancy (occurring in up to 25% of healthy pregnancies). However, if you experience heavy bleeding, bright red blood, or cramping, contact your healthcare provider immediately.
How does this calculator estimate risk?
It combines daily probability data from large population studies with specific multipliers for your age, history, and ultrasound findings. See the Methodology section below for the exact data sources.
Methodology and sources
This calculator estimates the chance of miscarriage from the entered gestational age up to 20 weeks. It is a statistical estimate. It does not diagnose miscarriage or confirm viability.
Inputs used
- Maternal age (years)
- Gestational age (week and day)
- Ultrasound status, and whether a fetal heartbeat was seen
- Optional fetal heart rate (bpm), only used when heartbeat is marked as seen
- Previous miscarriages and previous live births
- Bleeding (yes/no)
- Height and weight to estimate BMI (optional). Imperial and metric are converted internally.
How the estimate is calculated
-
Baseline risk from gestational age:
- If "heartbeat detected" is selected, the calculator uses a lower baseline curve by gestational week, then applies a small per-day decrease. For example, the baseline is about 1.6% at 8w0d, then about 0.05 percentage points lower per day (with a floor).
- If heartbeat is not selected, the calculator uses a higher baseline lookup table by week and day. For example, the table baseline is about 13.5% at 6w0d and about 5.2% at 8w0d (before any other inputs are applied).
- This reflects that risk is generally lower once a live fetus is detected on ultrasound, compared with pregnancies of unknown viability. [1]
-
Convert risk percent to odds, apply a multiplier, then convert back to percent:
- odds = p / (100 - p)
- newOdds = odds * multiplier
- newP = 100 * newOdds / (1 + newOdds)
-
Maternal age adjustment (always applied):
- The calculator maps age to a multiplier using anchor points and linear interpolation between them.
- Example multipliers used in this implementation: age 35 uses 1.3, age 40 uses 2.0, age 42 uses 3.0, and age 45+ uses 4.5. Age 20 and under uses 0.8.
- Maternal age is a consistent risk factor for miscarriage in large population datasets. [2][5]
-
Pregnancy history adjustment:
- Previous miscarriages increase the odds using stepwise multipliers. Example multipliers used in this implementation: 1 prior miscarriage uses 1.25, 2 prior miscarriages uses 1.5, and 3+ uses 2.2. Prior loss is consistently associated with higher subsequent loss risk in population data and clinical reviews. [3][4][5]
- Previous live births reduce the odds using stepwise multipliers. Example multipliers used in this implementation: 1 prior live birth uses 0.8, and 2+ uses 0.7 (capped benefit). This is an implementation choice. Some large datasets stratify fetal loss risk by parity. [2]
-
BMI adjustment (optional):
- If height and weight are present, BMI is calculated, then grouped into simple bands.
- Example multipliers used in this implementation: BMI under 18.5 uses 1.2; BMI 30 to 34.9 uses 1.3; BMI 35 to 44.9 uses 1.6; BMI 45+ uses 1.9; otherwise 1.0.
- Obesity is commonly listed as a risk factor for early pregnancy loss in clinical reviews. The specific BMI cutoffs and multipliers above are simplified for usability. [5]
-
Bleeding adjustment:
- If bleeding is selected, a multiplier is applied.
- Example multipliers used in this implementation: 2.5 if heartbeat is not selected, and 1.5 if heartbeat is selected.
- First-trimester bleeding is common and is associated with higher loss risk in many studies, but risk depends on severity, pain, and ultrasound findings. [1][5]
-
Fetal heart rate adjustment (optional, only when heartbeat is selected):
- If the entered heart rate is below a simplified threshold for the gestational week, the odds are increased.
- Thresholds used in this implementation: under 100 bpm at 6 weeks or earlier is treated as slow; under 120 bpm at 7 weeks and later is treated as slow.
- Example multipliers used in this implementation: if slow, odds are multiplied by 3.0; if not slow, odds are multiplied by 0.8 (reassuring effect).
- Slow embryonic heart rate in early pregnancy has been associated with higher loss risk in observational studies. [6]
-
Clamp and display:
- The final risk is clamped to 0.1% to 99.0%.
- "Chance of continuing" is shown as 100% minus risk.
- The bar segments animate by setting their CSS widths to the final percentages.
- The "or about 1 in N" line is a rounded fraction based on the displayed percentage.
Guardrails in the calculator
- If gestational age is 20 weeks or more, the calculator stops and shows a redirect message to a stillbirth risk calculator. US clinical references commonly define spontaneous abortion (miscarriage) as loss before 20 weeks of gestation. [1][5]
- If ultrasound is marked "yes", gestational age is 11 weeks or more, and heartbeat is marked "no", the calculator stops and shows a safety message instead of a percentage. This is a guardrail. Clinical diagnosis of non-viability is normally based on ultrasound measurements and established criteria, not gestational age alone. [7]
Limitations
- Gestational dating error can materially change the estimate, especially in early weeks.
- The baseline tables and the size of each adjustment are simplified for usability. They should not be treated as patient-specific risk.
- The bleeding input is binary. Real-world risk depends on bleeding amount, duration, pain, and ultrasound findings.
- Fetal heart rate thresholds are simplified. They are not diagnostic cut-offs.
- The calculator applies multipliers even when heartbeat is marked as seen. Real-world interactions between factors can be more complex than a single multiplicative model.
Sources
- [1] First Trimester Bleeding: Evaluation and Management . American Family Physician (American Academy of Family Physicians). 2019.
- [2] Maternal age and fetal loss: population based register linkage study . BMJ. PubMed (PMID: 10864550). 2000.
- [3] Recurrent miscarriage: are three miscarriages one too many? Analysis of a Scottish population-based database of 151,021 pregnancies . Bhattacharya S, Townend J, Bhattacharya S. Eur J Obstet Gynecol Reprod Biol. 2010. PubMed (PMID: 20207064).
- [4] Risks of repeated miscarriage . PubMed (PMID: 16466430).
- [5] Early Pregnancy Loss (Spontaneous Abortion) . StatPearls (NCBI Bookshelf, National Library of Medicine). Updated 12 Oct 2023.
- [6] Predicting first-trimester spontaneous abortion. Ratio of mean sac diameter to crown-rump length compared to embryonic heart rate . Tadmor OP, Achiron R, Rabinowiz R, Aboulafia Y, Mashiach S, Diamant YZ. J Reprod Med. 1994. PubMed (PMID: 7932400).
- [7] Diagnostic criteria for nonviable pregnancy early in the first trimester . Doubilet PM, Benson CB, Bourne T, Blaivas M, et al. N Engl J Med. 2013. PubMed (PMID: 24106937).
- Ectopic pregnancy and miscarriage: diagnosis and initial management . NICE guideline (NG126). National Institute for Health and Care Excellence (NICE). Published 17 Apr 2019. Last updated 23 Aug 2023.
- Early Pregnancy Loss: ACOG Practice Bulletin, Number 200 . Obstetrics and Gynecology. 2018 Nov;132(5):e197-e207. PubMed (PMID: 30157093).
- Miscarriage risk for asymptomatic women after a normal first-trimester prenatal visit . Obstetrics and Gynecology. 2008 Mar;111(3):710-4. PubMed (PMID: 18310375).
Support if you have experienced a loss
Reading about miscarriage, stillbirth, or infant loss can be difficult. If you have experienced a loss, you do not have to use this calculator or read the statistics. You may find it more helpful to talk with your care team or a support organization.
In the United States, groups such as:
offer information and bereavement support. If you are elsewhere, your local health service or a pregnancy and baby loss charity may be able to guide you to support in your region.
Medical disclaimer
The information and calculators on this site are educational tools only. They provide statistical estimates based on published research and the details you enter.
They cannot diagnose, predict what will happen for you, or replace personalized advice from a licensed health care professional who knows your full history. Always talk with your doctor, midwife, or other qualified clinician before making decisions about your health, fertility, or pregnancy.
Never ignore, avoid, or delay seeking professional medical advice because of something you read here or a result you see in a calculator. If you think you may be having a medical emergency, call 911 in the United States or your local emergency number.
