Reviewed by Dr. Sony Sherpa, MBBS, MD on Dec 22, 2025
Estimate your likelihood of twins based on age, family history (maternal side), height/BMI, ethnicity, prior pregnancies, fertility treatment, and past twins. Results show a baseline risk with a fraternal (dizygotic) vs identical (monozygotic) split, using population studies.
Key points
- Fraternal (dizygotic) twins happen when two eggs are fertilized. Their odds vary with factors like maternal age, family history on the maternal side, prior pregnancies, height/BMI, ethnicity, and fertility treatment.
- Identical (monozygotic) twins come from one embryo splitting. Rates are relatively stable across groups and are less influenced by age or family history.
- Single-embryo transfer (SET) in IVF lowers twin odds; transferring multiple embryos increases twin odds.
- Your result is a population-based estimate. Only ultrasound can confirm twins.
What affects the odds?
- Maternal age: Twin rates (especially fraternal) tend to rise through the early–mid 30s.
- Maternal family history: A mother with female relatives who had fraternal twins may have higher odds.
- Parity/prior twins: Previous pregnancies - and especially previous fraternal twins - are linked with higher odds.
- Body size: Taller body size and higher BMI have been associated with more fraternal twinning.
- Ethnicity: Twin rates differ by population in published registries.
- Fertility treatment: Ovulation-inducing meds and transferring multiple embryos can raise twin odds. Discuss embryo-transfer policies with your clinic.
Important: None of these factors “cause” twins on their own. They shift probabilities only.
FAQ
Do identical twins run in families?
Identical twinning is mostly random and not strongly tied to family history. Fraternal twins are the type more associated with maternal family history.
Does IVF always mean twins?
No. Many clinics recommend single-embryo transfer (SET). Twin likelihood depends on your clinic’s protocol and number of embryos transferred.
Can high hCG prove twins?
Higher hCG can occur with twins but is not diagnostic. Only ultrasound can confirm twins.
Do twins skip a generation?
That’s a myth. What matters most for fraternal twinning is ovulation of multiple eggs - which can run on the maternal side.
Methodology and sources
What this estimates
This calculator estimates the chance that a single pregnancy will be twins. It does not estimate your chance of getting pregnant or your chance of twins across your whole life.
Natural twin chance
The model starts with an average chance of twins in naturally conceived pregnancies. This is split into two parts: fraternal twins (dizygotic, DZ) and identical twins (monozygotic, MZ). The DZ baseline is set at about 1.2 percent of pregnancies. The MZ baseline is set at about 0.35 to 0.4 percent of pregnancies, which is fairly stable worldwide and mostly does not depend on age or family history.
Factors that adjust the DZ chance
The DZ part of the risk is then adjusted up or down using published research. The main factors are:
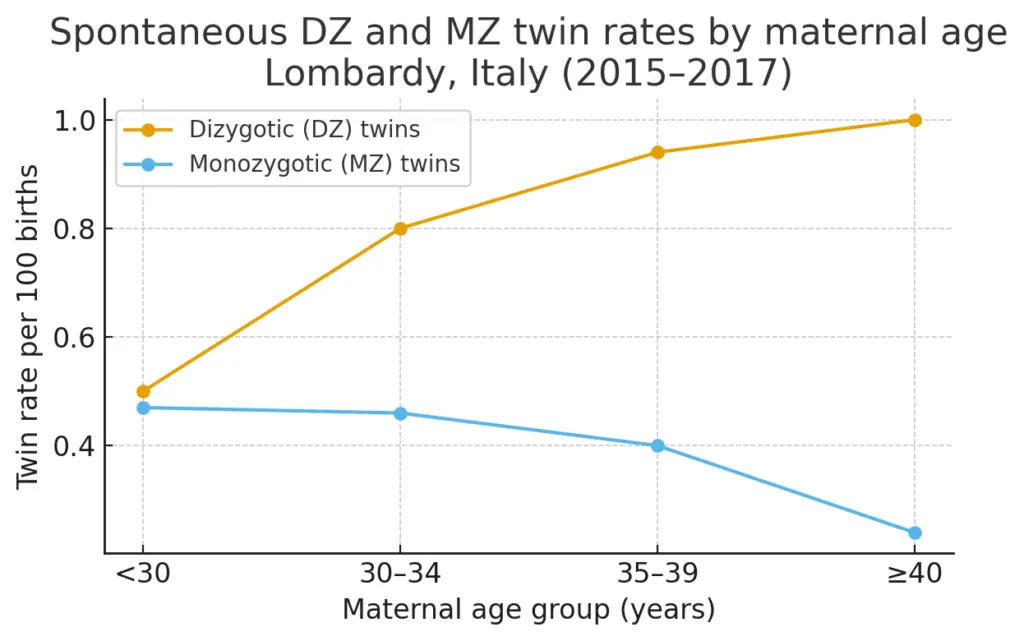
- Maternal age: DZ twins are most common in the early to mid 30s. The calculator increases the chance in that age range and lets it drop again in the late 30s and 40s.
- Prior births (parity): Having had several previous births slightly raises DZ twinning rates. The effect is capped so it does not grow without limit at very high parity.
- Maternal family history: A history of twins on the mother's side suggests a tendency to release more than one egg. The calculator raises the DZ chance if this is present.
- Height and body mass index (BMI): Taller height and higher BMI are linked with somewhat higher DZ twinning rates. Shorter stature and very low BMI are linked with slightly lower rates.
- Ethnicity group: Some population groups have naturally higher or lower DZ rates than the global average. The model nudges the DZ chance up or down to reflect these patterns.
- Previous twins: Having had spontaneous twins before is a strong signal of higher DZ chances in future pregnancies, so this factor is given extra weight.
The MZ part of the risk is kept almost constant, because identical twins usually happen at a low background rate that is less affected by these factors.
Fertility treatment scenarios
When you select a fertility treatment, the calculator starts from typical twin rates reported for that type of care and then blends them with the natural baseline and your age:
- Ovulation induction medicines and IUI with stimulation: Trials of clomiphene, letrozole and gonadotropins with IUI show twin and higher order multiple rates around 6 to 15 percent in many settings. The tool maps the "ovulation induction" and "IUI with stimulation" options into this band and adjusts gently for age.
- IVF with single embryo transfer (SET): With modern SET policies, most twin pregnancies come from one embryo splitting. Twin rates are usually around 1 to 3 percent. The calculator keeps the DZ chance near zero and keeps a small MZ component.
- IVF with two embryos transferred (DET): Transferring two embryos creates a higher DZ twin chance, often around 20 to 30 percent in younger patients. The model reflects this but still limits results to a realistic range for older ages.
The "Typical range" shown under the treatment result gives a rough band around the main estimate (about plus or minus 20 percent) to show that clinics, doses and protocols differ.
How the model combines factors
For natural conception, the calculator multiplies the DZ baseline by the age, parity, family history, height, BMI, ethnicity and prior twin factors, then adds the MZ baseline. For treatment scenarios, it replaces the DZ part with a typical rate for that treatment and keeps a small MZ component that fits the technique. All results are kept within plausible upper and lower bounds so that extreme combinations of answers do not produce unrealistic percentages.
Missing or average values
If height or weight are left blank, the calculator uses average values. This mainly affects the BMI adjustment and usually only changes the final percentage by a small amount.
Limits of the estimate
This model uses population averages. It cannot account for details such as exact drug doses, embryo quality, embryo stage, genetic testing, clinic policies, or specific health conditions. Real world twin rates for you and your clinic may be higher or lower than the estimate.
Disclaimer
This tool is for general education only and is not medical advice. It does not replace counselling with your fertility specialist or maternity care team. Always discuss your own situation and risks with your clinician.
Main sources
Key references include large studies of global twinning patterns, reviews of factors that affect fraternal twinning, and trials and registry data on multiple pregnancy rates with fertility treatment, such as:
- Monden C, Smits J. Twinning across the developing world. Human Reproduction, 2021. (Comprehensive global study on twinning rates by region).
- Hoekstra C, et al. Dizygotic twinning. Human Reproduction Update, 2008. (Review of factors like height, BMI, and genetics).
- Reddy UM, et al. Relationship of maternal body mass index and height to twinning. Obstetrics and Gynecology, 2005.
- Diamond MP, Legro RS, et al. AMIGOS trial (Treatment rates). New England Journal of Medicine, 2015.
Medical disclaimer
The information and calculators on this site are educational tools only. They provide statistical estimates based on published research and the details you enter.
They cannot diagnose, predict what will happen for you, or replace personalized advice from a licensed health care professional who knows your full history. Always talk with your doctor, midwife, or other qualified clinician before making decisions about your health, fertility, or pregnancy.
Never ignore, avoid, or delay seeking professional medical advice because of something you read here or a result you see in a calculator. If you think you may be having a medical emergency, call 911 in the United States or your local emergency number.
